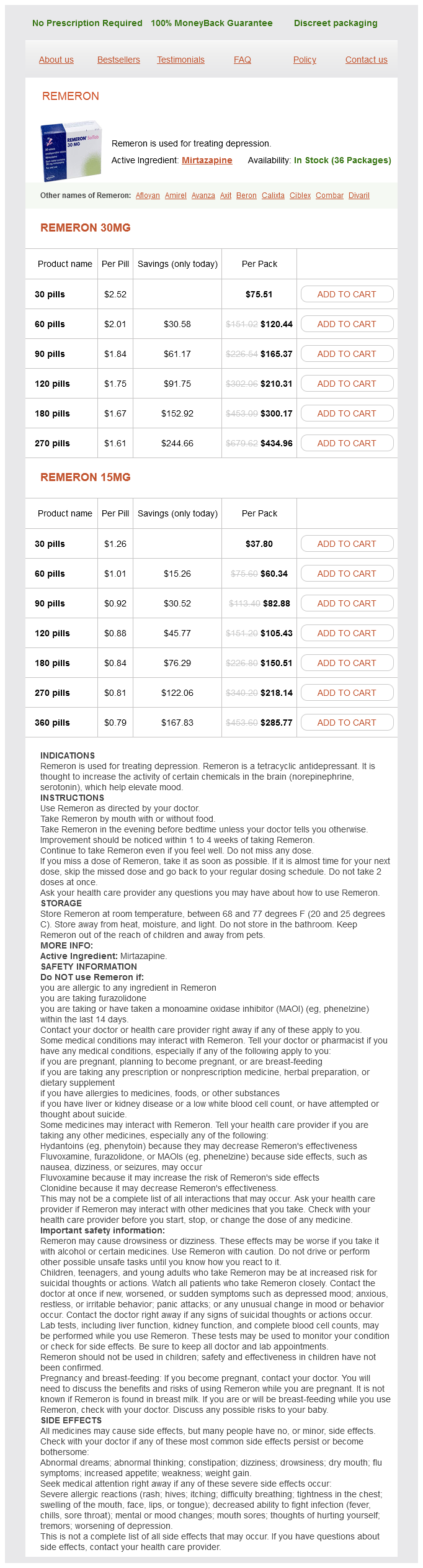
Remeron 30mg
- 30 pills - $75.51
- 60 pills - $120.44
- 90 pills - $165.37
- 120 pills - $210.31
- 180 pills - $300.17
- 270 pills - $434.96
Remeron 15mg
- 30 pills - $37.80
- 60 pills - $60.34
- 90 pills - $82.88
- 120 pills - $105.43
- 180 pills - $150.51
- 270 pills - $218.14
- 360 pills - $285.77
Remeron dosages: 30 mg, 15 mg
Remeron packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
In stock: 985
Only $0.75 per item
Description
The advantages of such long-term postnatal treatment in newborns 31 · Toxoplasmosis 1021 Table 31-20 Long-Term Outcomes From Three Cohort Studies of Children With Congenital Toxoplasma Infection treatment 2 degree burns remeron 15 mg cheap, Detected Through the French Prenatal Screening Program and Treated for 1 Year After Birth Berrébi et al461 Study period and location Number of patients Median length of follow-up (years) Asymptomatic infection at the last examination Non-ocular lesions Retinal lesions At the last examination 1985-2005, Toulouse 107 8 (1-20) 79 (74%) 6 (5%) 28 (26%) Unilateral visual impairment: 6 (21%) No bilateral impairment Birth: 11 (39%) <5 years: 24 (55%) <10 years: 27 (96%) Faucher et al428 1995-2010, Marseille 127 4 96 (76%) 11 (9%) 24 (19%) Unilateral visual impairment: 7 Bilateral visual impairment: 1 Birth: 11 <2 years: 18 (75%) <5 years: 22 (92%) Wallon et al136 1988-2001, Lyon 327 6 (interquartile range, 3-10) 232 (71%) 35 (11%) 79 (24%) Unilateral visual impairment: 24 (30%) No bilateral impairment First month: 9 (11%) <1 year: 38 (48%) <2 years: 46 (58%) <5 years: 60 (76%) <10 years: 75 (95%) Time of detection of first lesions with subclinical lesions need to be evaluated through carefully randomized studies. In the meantime, consideration must be given to reducing the constraints of and any harm that may be caused from such treatment by reducing its length in these nonseverely infected children. Outcome variables are the age at which new retinochoroidal lesions occur, neurologic developments, the anxiety levels of parents, and the quality of life of parents and children. Their attention should be drawn to the risk of false-positive test results and to the danger of misinterpreting residual IgM or low-avidity antibodies as signs of acute infection (see "Diagnosis of Maternal Infection"). Reference centers or groups should be available and their expertise requested to assess the risks for the fetus whenever atypical findings or a suspicion of infection are detected. Costs for follow-up testing should also be included in planning, as part of this option. Sufficient funding should also be available for educational material and campaigns and for the training of perinatal care providers, who should be able to give accurate advice on how a pregnant woman with a negative test can avoid infection, according to her level of risk and sociocultural profile. An inability to provide clear answers to their questions on risky or risk-free behaviors may be a source of stress in pregnant women who have been identified as susceptible. Option 1 A single test, before pregnancy or during the first trimester of pregnancy in women who are not known to be immune, is useful in terms of primary prevention because it discerns those who are susceptible to infection and need to be educated on its avoidance. It also promotes the collection of relevant epidemiologic data, such as time and geographic trends in the prevalence of Toxoplasma infection among pregnant women in different age groups, and the investigation of factors involved in past infection in women of different socioeconomic and cultural backgrounds. Constraints include the timing of the test, which should be performed as early as possible in pregnancy-or ideally before pregnancy-to allow the timely adoption of healthy, risk-free behaviors. When the result is positive, an early test also facilitates the exclusion of a perigravidic infection. Requirements for testing include the availability of high-performance tests that # References Option 2 the provision of a second test during the third trimester of pregnancy, or at delivery, for women who tested negative at the first test allows the identification of those who seroconverted during pregnancy, and the detection of Toxo plasma infection in their children. However, it also increases the technical constraints, in terms of test performance and the interpretation of their results in pregnant women and newborns, and the need for reliable reference centers or groups to be available to counsel obstetricians and pediatricians, who should be provided with criteria and guidelines for treatment, despite the uncertainty regarding the impact of postnatal treatment on the reduction of long-term ocular lesions. Option 3 Any additional testing during pregnancy offers the opportunity to detect incident maternal infections and to attempt to prevent transmission to the fetus by antenatal treatment. Retesting is performed at 3-monthly or monthly intervals according to the clinical settings. More frequent testing increases the costs of screening but might also increase its efficacy by expanding the opportunities of implementing prenatal treatment within 21 days of infection and thus reducing the risks4,491 and the severity88,687 of a congenital infection. However, any economic assessment of such procedures is limited by the lack of knowledge on the extent to which treatment reduces the proportion of disease compared with no treatment. Decision analysis is an ideal tool that takes into account the magnitude of disease in a local population and can hypothesize the proportion that can be prevented.
Gum Ivy (English Ivy). Remeron.
- Are there safety concerns?
- Dosing considerations for English Ivy.
- What is English Ivy?
- Chronic bronchitis.
- What other names is English Ivy known by?
- How does English Ivy work?
- Coughs; spasms; gout; arthritis-like pain; diseases of the liver, spleen, and gallbladder; burns; calluses; nerve pain; and ulcers.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96474
By age 6 months symptoms 28 weeks pregnant discount remeron 15 mg without a prescription, T cells bearing V9 V2 segments become predominant and remain so during adulthood,708 probably because of their preferential expansion in response to ubiquitous antigen(s), such as endogenous bacterial flora. In contrast with freshly isolated neonatal T cells, activation and propagation of these fetal and neonatal T cells in culture. The capacity of neonatal T cells for cytokine production is also markedly reduced under some conditions, but not all. T-cell response to alloantigens can also be detected in newborns after in utero irradiated red blood cell transfusions from unrelated donors. Another indication that neonatal T cells can mediate allogeneic responses is the fact that blood transfusions rarely induce graft-versus-host disease in the neonate. Rare cases of persistence of donor lymphocytes and of graft-versus-host disease have developed after intrauterine transfusion in the last trimester as well as in transfused premature neonates, however. Skin test reactivity to common antigens, such as Candida, streptokinase-streptodornase, and tetanus toxoid, usually is not detectable in neonates. Such deficiencies may account, at least in part, for diminished skin reactivity in the neonate after specific sensitization or after intradermal injection with T-cell mitogens. Several studies suggest that fetal T cells have become primed to environmental or dietary protein allergens as a result of maternal exposure and transfer to the fetus. In addition, many of these studies used antigen extracts rather than defined recombinant proteins or peptides, and these may have nonspecific stimulatory effects. Together, this suggests that fetal sensitization to foreign proteins may be relatively inefficient, particularly when exposure is temporally limited. Whether this reflects relatively inefficient maternal-fetal transfer of protein antigens or intrinsic limitations of the fetus for antigen presentation and T-cell priming, or both, is unclear. Even if it is 4 · Developmental Immunology and Role of Host Defenses in Fetal and Neonatal Susceptibility to Infection 143 assumed that the capacity for fetal T cells to be primed by foreign antigens is similar to that of antigenically naïve adult T cells, the immune response to maternally derived foreign vaccine proteins by fetal T cells would be expected to be poor compared with the maternal response because antigen probably enters into the fetal circulation with little if any accompanying activation of the innate response required for efficient T-cell activation. Growing evidence, however, suggests that fetal T-cell sensitization can occur in cases of antigen exposure resulting from chronic infection of the mother with parasites or viruses: Parasite (schistosomal, filarial, and plasmodial) antigen-specific cytokine production by peripheral blood lymphocytes, probably of T-cell origin, was detectable at birth in infants without congenital infection who were born to infected mothers. Although maternalto-fetal transfer of leukocytes, particularly T cells, occurs, their number in the fetus is very low (usually < 0. With severe infections in the first trimester, a direct deleterious effect on T-cell development is possible. T cells from infants and children with congenital toxoplasmosis, however, retain the ability to respond to alloantigen, mitogen, and, in one case, tetanus toxoid. Whether this reflects limitations in antigen processing, T-cell activation and co-stimulation, or proliferation 4 · Developmental Immunology and Role of Host Defenses in Fetal and Neonatal Susceptibility to Infection 145 and differentiation remains unclear. In any case, these results suggest that infants tend to develop less robust Th1 responses and polyfunctional cytokine responses to inactivated vaccines during their primary immunization series than adults receiving booster vaccines, but, compared with adults, infants may preferentially accumulate central memory T cells, which are associated with relatively durable immune responses (see "Overview of Memory T Cells").
Specifications/Details
As with maternal rubella treatment using drugs remeron 30 mg buy cheap, congenital infection must be confirmed by laboratory tests. In contrast to maternal rubella, attempting to isolate rubella virus in tissue culture is a valuable tool for diagnosing congenital rubella in newborns. In older children in whom virus shedding has ceased from other sites, virus may be isolated from cataractous lens tissue. First, cord serum can be assayed for the presence of rubella-specific IgM antibody. False-positive results may occur, however, because of rheumatoid factor or incomplete removal of IgG (largely maternal), depending on the techniques used. A few newborns with stigmata of congenital rubella may not have detectable levels of rubella-specific IgM in sera taken during the first days of life, and some infections may go undiagnosed if infection occurred late in pregnancy because it is theoretically possible that there was inadequate time for the fetus to produce detectable levels of specific IgM antibodies by the time of delivery. Persistence of IgG antibody at this age, especially in high titer, is presumptive evidence of intrauterine infection with rubella virus. Sera should be drawn when the infant is 3 months and then 5 to 6 months of age, with a repeat specimen at 12 months of age if necessary. Important limitations of this method are the delay in diagnosis and the fact that rubella infections occurring after birth may be mistaken for congenital infections. Confirming the diagnosis, counseling about the risks of infection of and damage to the fetus, and discussing courses of action, including the use of immunoglobulin and consideration of termination of pregnancy, require a thorough understanding of the natural history and consequences of rubella in pregnancy. In the case of congenital infection, the emphasis is on diagnosis and acute and longterm management. This finding is not surprising because extensive viral replication is demonstrable 1 week or more before symptoms appear, with initial replication probably beginning even earlier. The amount of antirubella antibody in commercial immunoglobulin preparations is variable and unpredictable; specific hyperimmunoglobulin preparations are unavailable. Fetal infection occurred when immunoglobulin was administered to the mother in what seemed to be adequate amounts soon after exposure. Another disadvantage of immunoglobulin is that it may eliminate or §d References 2, 13, 165, 289-294, 296, 333, 334, 336, 338, 402, 405. If maternal blood is negative for IgM (IgM-), the IgG results determine if the woman is seropositive (immune) or seronegative (not immune). If not immune, the woman should be retested monthly for seroconversion until the end of the fifth month of pregnancy. If the maternal blood is positive for IgM (IgM+) and IgG (IgG+), the next step would be an IgG avidity assay on the same blood sample to estimate the time of infection. If the results remain the same (IgM+ IgG-), the IgM result is considered nonspecific, indicating that the woman has not been infected; however, she is seronegative and should be followed until the end of the 5th month. If the woman has seroconverted (IgM+ IgG+), recent primary infection is confirmed, and a prenatal diagnosis should be made if the woman wishes to continue her pregnancy.
Syndromes
- Enlarged prostate
- May have a rough texture (like a wart)
- Fatigue
- ESR
- Polymerase chain reaction (PCR) of CSF
- How long has it lasted?
- What other symptoms do you have?
Related Products
Additional information:
Usage: q.d.
Tags: remeron 30 mg buy otc, buy remeron 30 mg without a prescription, remeron 15 mg purchase with amex, 30 mg remeron purchase with amex
9 of 10
Votes: 231 votes
Total customer reviews: 231
Customer Reviews
Yussuf, 65 years: Outbreaks of pneumonia in neonates have been reported with echovirus 11 and parechovirus 1. Lactation ceases when suckling stops; therefore any behavior that reduces the amount of suckling by the infant initiates weaning or the end of lactation. Descriptions of "umbilical sepsis" and "acute interstitial hepatitis" recorded by Morison40 seem to indicate that his patients had acquired bacterial infections of umbilical vessels with widespread extension into portal tracts.
Onatas, 38 years: Second attacks of zoster were historically considered unusual, although recent evidence suggests that the rates are comparable to those of the first episode in immunocompetent individuals. Asymptomatic bacteriuria, cystitis, or pyelonephritis occurs in 6% to 8% of women during pregnancy. In Massachusetts and New Hampshire, unlike other states in the United States, all newborns are tested for toxoplasmosis.
Goran, 42 years: This child had pneumonia when 3 weeks of age, but general neurologic improvement occurred. The acute phase specimen should be obtained as soon as possible after onset of the rash, ideally within 7 days. If IgG avidity is high and IgG titers are If IgG avidity is high and IgG titers are stable, stable, infection occurred at least 3 infection occurred at least 3 months earlier.
Hjalte, 34 years: Lazzarotto T, Spezzacatena P, Pradelli P, et al: Avidity of immunoglobulin G directed against human cytomegalovirus during primary and secondary infections in immunocompetent and immunocompromised subjects, Clin Diagn Lab Immunol 4:469-473, 1997. Birenbaum E, Handsher R, Kuint J, et al: Echovirus type 22 outbreak associated with gastro-intestinal disease in a neonatal intensive care unit, Am J Perinatol 14:469, 1997. Ndir I, Gaye A, Faye B, et al: Seroprevalence of toxoplasmosis among women having spontaneous abortion and pregnant women following in a center of health up-town in Dakar, Dakar Med 49:5-9, 2004.
Lars, 63 years: If no lesions develop in the neonate by the time the mother is noninfectious, both may be sent home. Using in situ hybridization for Ureaplasma on lung autopsy tissue from 7 infants with positive cultures and 7 infants with negative cultures for Ureaplasma from the lower respiratory tract, Benstein and coworkers95 found all 7 culture-positive infants were positive for Ureaplasma by in situ hybridization; 2 of the culture-negative infants were positive by in situ hybridization. Kempe A, Rösing B, Berg C, et al: First-trimester treatment of fetal anemia secondary to parvovirus B19 infection, Ultrasound Obstet Gynecol 29:226-228, 2007.